Editor’s note: By mistake, an unfinished version with a huge cut and paste error was originally published. That is entirely my fault. It has been fixed, and this is the correct version. Sorry about that.
 It’s getting depressing. It’s as though nothing ever changes, and maybe nothing ever does. Regular readers probably remember the Disneyland measles outbreak four years ago. As bad as that outbreak was, however, it was an outbreak that made the impossible possible; in its aftermath, spearheaded by Sens. Richard Pan and Ben Allen, California passed SB 277, a law that eliminated nonmedical exemptions to school vaccine mandates. SB 277 was approved by the California legislature in June 2015 and signed into law by Governor Jerry Brown on June 30, 2015. The new law took full effect in the 2016-2017 school year, and it has worked. Nonmedical exemptions have plummeted. That’s not to say that the law is perfect. Unfortunately, there’s a huge loophole in that any physician can write a letter in support for a medical exemption. Not surprisingly antivaxers have taken advantage of that weakness in the law, namely that there is no overriding governmental body that reviews and approves requests for medical exemptions, as there is in, for example, West Virginia, where requests for medical exemptions are reviewed by an Immunization Officer, who determines if they are appropriate “based upon the most recent guidance from the Advisory Committee on Immunization Practices (ACIP), the American Academy of Pediatrics (AAP), and the American Academy of Family Physicians (AAFP) with respect to medical contraindications or precautions for each vaccine”.
It’s getting depressing. It’s as though nothing ever changes, and maybe nothing ever does. Regular readers probably remember the Disneyland measles outbreak four years ago. As bad as that outbreak was, however, it was an outbreak that made the impossible possible; in its aftermath, spearheaded by Sens. Richard Pan and Ben Allen, California passed SB 277, a law that eliminated nonmedical exemptions to school vaccine mandates. SB 277 was approved by the California legislature in June 2015 and signed into law by Governor Jerry Brown on June 30, 2015. The new law took full effect in the 2016-2017 school year, and it has worked. Nonmedical exemptions have plummeted. That’s not to say that the law is perfect. Unfortunately, there’s a huge loophole in that any physician can write a letter in support for a medical exemption. Not surprisingly antivaxers have taken advantage of that weakness in the law, namely that there is no overriding governmental body that reviews and approves requests for medical exemptions, as there is in, for example, West Virginia, where requests for medical exemptions are reviewed by an Immunization Officer, who determines if they are appropriate “based upon the most recent guidance from the Advisory Committee on Immunization Practices (ACIP), the American Academy of Pediatrics (AAP), and the American Academy of Family Physicians (AAFP) with respect to medical contraindications or precautions for each vaccine”.
As a result, medical exemption rates have increased, thanks to an increase in medical exemption requests, some likely organic from parents who found it easier to claim nonmedical exemptions than going to the trouble of claiming a medical exemption, but also due to bogus medical exemptions on sale from a cottage industry of antivaccine quacks like Dr. Bob Sears, who blazed the trail.
Unfortunately, we’re in the midst of multiple new measles outbreaks, the largest occurring in Washington, across the Columbia River from Portland, Oregon. As a result, the same battles from 2015 are taking place in 2019, this time with antivaxers rallying in a state with a major measles outbreak to oppose a bill that would eliminate personal or philosophical exemptions to requirements families immunize their children against measles, mumps, and rubella (MMR), led by—who else?—Robert F. Kennedy, Jr. and the usual cast of characters. This bill isn’t even as comprehensive as SB 277 in that it wouldn’t eliminate religious exemptions, but antivaxers are still fighting it with all they have. Of course, you can predict what will happen if this bill passes; antivaxers will all get religion.
As history repeats itself—whether this time as farce or not, I’ll leave the reader to decide, although arguably everything antivaxers do is infused with farce—there are other elements that keep repeating, in particular, the claim that measles is “not that big a deal” or “just a childhood disease.” You might remember the brain dead argument that because there was an episode of The Brady Bunch that made a joke about the kids getting measles, it must mean that doctors didn’t think measles was dangerous back then. It is, as I like to call it, the Brady Bunch fallacy. But is this true? The answer, obviously, is no.
The dangers of measles, take one: SSPE
Of course, we’ve discussed the dangers of measles before here on SBM many times. For instance, the complications of pneumonia, encephalitis, and perhaps the most feared complication of measles, subacute sclerosing panencephalitis (SSPE), a universally fatal complication in which the measles virus lies dormant in the brain, only to reactivate on average 7-10 years following the measles infection. As Steve Novella described it, SSPE leads to “severe brain inflammation. SSPE causes widespread damage to the brain. It usually starts subtly with changes in behavior, problems at school, difficulty walking, and muscle twitching. As the disease progresses it causes seizures of increasing frequency and severity, and progressive dementia. Eventually the disease leads to coma and death, on average 1-2 years from onset of symptoms. The disease is universally fatal and without any cure.” The risk of SSPE after measles had been estimated at one in 100,000, but it turns out that children who get the measles before age 5 could have as high as a one in 1,387 chance of developing SSPE, and kids who get the measles before age 1 could have a one in 609 chance.
It turns out that a “rare” complication of measles is not as rare as had previously been believed.
The dangers of measles, take two: a new study
Basically everyone, even the antivaccine movement, concedes that the measles vaccine is highly effective at preventing the measles. Actually, there are a few who don’t, but most simply try to argue that measles isn’t deadly and that therefore the fantastical “risks” ascribed to the vaccine by antivaxers (autism, neurodevelopmental disorders, diabetes, sudden infant death syndrome, etc.) outweigh the benefits of presenting measles. Be that as it may, the point is that the main benefit of vaccinating for measles has generally been believed to be the not-insignificant benefit of preventing the measles and its attendant complications, including the most dreaded SSPE. However, a new body of evidence is developing that the benefits of preventing measles go beyond just preventing measles and its known complications. In fact, it turns out that vaccinating against measles lowers all-cause mortality among children.
A new study adds to the growing evidence that measles is even more harmful than traditionally thought, making measles vaccination even more important than believed. From Science Daily:
In the largest study to date on children in a low/middle income country, new research in Ghana finds that the timing of a measles vaccine in an overall vaccination schedule can have a profound impact on child survival rates beyond protecting against measles infection. The findings, published today in open access journal Frontiers in Public Health, suggest that measles vaccination in the recommended sequence may have made an important contribution towards achieving the Millennium Development Goal 4 of reducing child mortality.
Here’s the study. Basically, it followed yearly cohorts of children aged 9-23 months from 1996 to 2012. The study area was the Kassena-Nankana East and West Districts in the Upper East region of northern Ghana, which have an estimated population is 160,000 of whom about 8% of the current population is aged 9–23 months. The area is quite large, covering a land area of 1,675 km2. Its major health care facilities include a hospital that serves as a referral hospital to seven health centers, a private clinic, and over 40 Community Health Compounds located in rural communities and manned by trained nurses who provide basic health care as well as routine vaccinations. The area is mostly rural (80%) with the primary occupation being agriculture.
Before we get to the results, here’s some background on the current vaccination schedule in Ghana and its history that will help put those results into context. The current schedule in Ghana includes one dose of Bacille Calmette–Guerin (BCG) at birth, four doses of oral polio vaccine (OPV) (at birth, 6, 10, and 14 weeks), three doses of pentavalent (Penta) vaccine (at 6, 10, and 14 weeks), two doses of rotavirus at (6 and 10 weeks), three doses of pneumococcal vaccines (at 6, 10, and 14 weeks), two doses of measles (at 9 and 18 months), and one dose of yellow fever (at 9 months). Note that Penta vaccine (diphtheria, tetanus, pertussis, Haemophilus influenza type b, and hepatitis B) was introduced in January 2002 to replace diphtheria–tetanus–pertussis (DTP), and in May 2012, three additional vaccines, pneumococcal, rotavirus, and second dose measles vaccine (MV), were added to the vaccination schedule for 18-month-olds.
For this study, a total of 38,333 children were assessed for survival in relation to the measles vaccination status within the first 12 months from interview date and until 5 years of age, using Cox proportional hazards models. The findings were quite striking. In essence, measles vaccine (MV), after the third dose of diphtheria-tetanus-pertussis (DTP, or DTP3), is associated with a significant decrease in all-cause mortality in the children in this cohort.
With that background, here are the details:
Children not vaccinated with MV at enrollment had 38% higher risk of dying than those vaccinated with MV-after-DTP3 during 12 months of follow-up [HR = 1.38 (1.15–1.66)] (Table 2). When mortality was assessed from interview date until 5 years of age, measles-unvaccinated children had 22% higher risk of dying than children vaccinated with MV-after-DTP3 [HR = 1.22 (1.05–1.41)]. The size of the beneficial effect of MV did not change when we censored for measles deaths (Table S1 in Supplementary Material).
Stratifying the analysis by periods in which DTP and Penta were used, children without MV in the DTP period (1996–2001) had 30% higher risk of dying in the first 12 months of follow-up [HR = 1.30 (1.04–1.62)] than those who received MV-after-DTP3. In the Penta period (2002–2012), children without MV had 52% higher risk of dying during 12 months of follow-up than those who received MV after Penta3 [HR = 1.52 (1.12–2.05)] (Table 2). The risk associated with not receiving MV did not change when we censored for measles deaths (Table S1 in Supplementary Material). When the children were followed from the assessment date until they were 5 years old, children without MV during the DTP period had 10% higher risk of dying than those with MV after DTP3 [HR = 1.10 (0.92–1.32)]. In the Penta period, children without MV had 44% higher risk of dying than those who received MV after Penta3 [HR = 1.44 (1.13–1.84)] when they were followed from the assessment date until they were 5 years old. The risk of dying for MV-unvaccinated children was higher during the Penta period compared to the DTP period in the first 12 months after assessment of vaccination status (52 vs 30%) (P = 0.021), and with follow-up to 5 years of age (44 vs 10%) (P = 0.005).
The most important qualifier in the results discussed above is this: “The risk associated with not receiving MV did not change when we censored for measles deaths.” In other words, even though the measles vaccine protects against measles, it protects against more than just the measles. Those who didn’t die of the measles were still protected by the measles vaccine from other causes of death:
We, further, classified the MV-unvaccinated children into two groups; children who received other vaccines but not MV, and those who did not receive any vaccine (unvaccinated). The adjusted HR for those who received other vaccines except MV compared with MV-after-DTP3 vaccinated children was 1.42 (1.18–1.72) in the first 12 months after assessment of vaccination status and 1.24 (1.06–1.44) with follow-up to 5 years of age.
So basically, the measles vaccine was the key, with decreased mortality associated with its receipt after DPT3. The authors looked for potential confounding factors, such as “general improvement in the health-care delivery system, health literacy as well as infrastructure, which could have affected the mortality rates and also increased MV coverage.” They also conceded that the comparison group of no measles vaccine “may represent the population with no access or difficult access to vaccines or health care, hence have higher mortality in general.” However, they pointed out that they still observed much higher mortality among MV-unvaccinated children compared with MV-after-DTP3 in “both communities with nurses and control communities without nurses” and that the “difference between the two groups disappeared making it unlikely that the difference in mortality is primarily due to inherent weaknesses or frailty.”
Overall, the results of this study clearly demonstrate a nonspecific benefit to measles vaccination, but the mechanism is unclear, particularly given the inconsistencies noted with previous studies, which the authors freely discuss:
Our results point to a beneficial effect of MV on child survival. The 38% higher mortality for MV-unvaccinated children would correspond to 28% lower mortality for MV-vaccinated children. Considering that this estimate is probably conservative, this is consistent with other studies from developing countries which have reported mortality reductions in the range of 30–86% (3, 6). Other studies comparing mortality rates before and after the introduction of MV reported major reductions in mortality after the introduction of MV (3, 28–31). The data from the present study also supported that MV may have non-specific beneficial effects which go beyond protecting children from dying from measles infection.
Measles vaccination was associated with beneficial effect for both boys and girls before receiving any campaign vaccine (Table 4). However, after the campaigns, we found a significantly stronger beneficial effect of measles vaccination for boys, but not for girls. It is unclear why the beneficial effect is stronger for boys as many other studies reported stronger beneficial effects of measles vaccination for girls than boys. For example the SAGE review suggested that MV had a 40% (22–53%) stronger effect for girls than boys (6). However, some studies have suggested that OPV is associated with stronger beneficial effects for boys than for girls (32, 33). Hence, we recommend that future studies examine the sex-differential effect of measles vaccination on all-cause mortality before and after OPV or measles campaigns.
I noticed this sex-associated difference as well, because I remembered a study from 2015 that I discussed, which observed the same thing (a decreased mortality in children vaccinated against the measles that couldn’t be explained by just its effect on measles incidence) but with a more marked effect among girls. The hypothesis supported by the study was that measles infection causes an immunomodulation/immunosuppression that lasts around three years after the infection and that can lead to increased mortality from other infectious diseases. Other studies are less clear-cut in terms of a mechanism, but several studies show an association between vaccination against measles (and a few other diseases) with decreased all-cause mortality.
Vaccines: More powerful than believed?
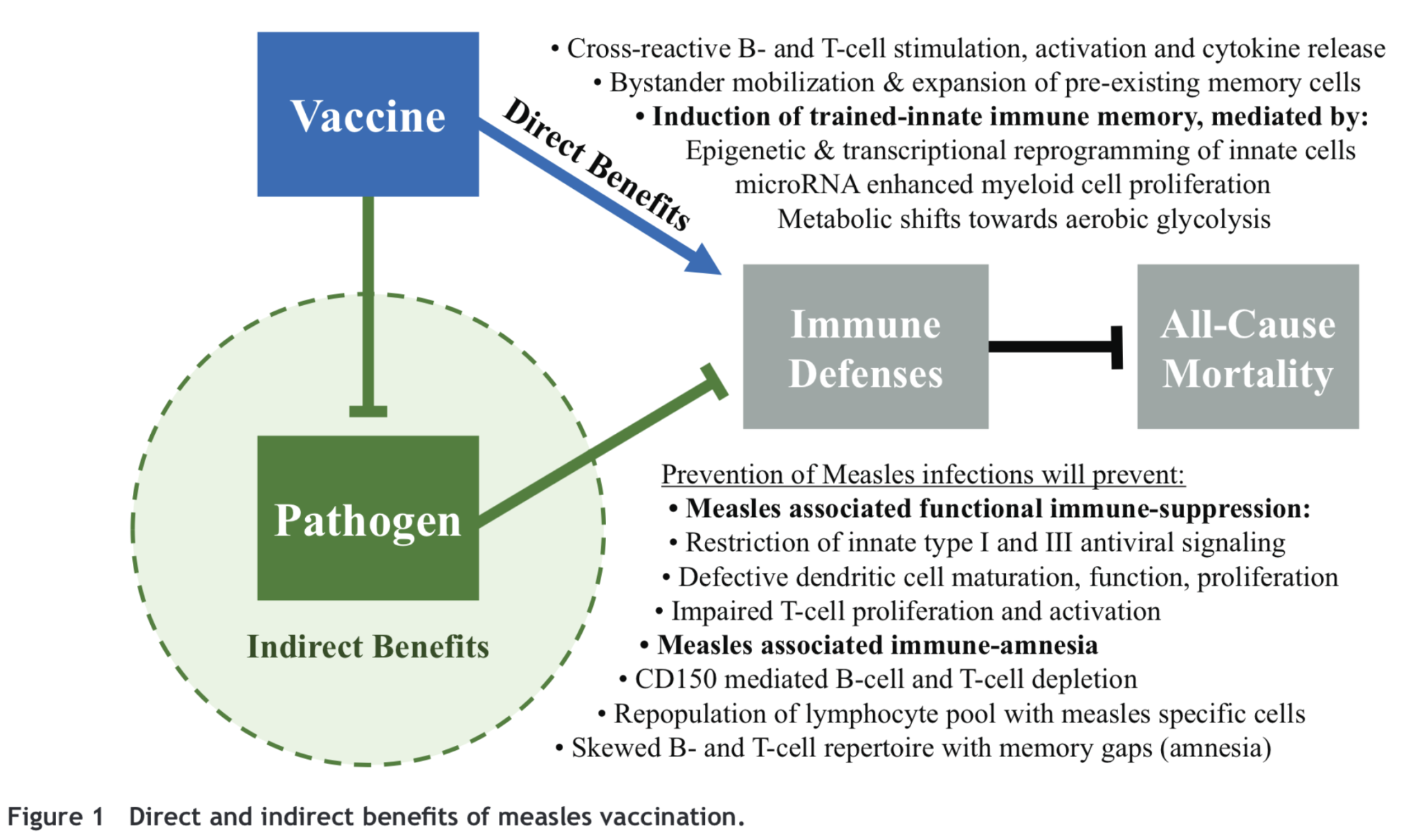
If “all” that vaccination did was to decrease deaths from infectious disease, they would still be the most effective preventative medicine ever conceived by the human mind, but it turns out that they might do even more than just prevent the diseases they are designed to prevent. Michael J. Mina hypothesized a mechanism in 2017:
A lot of this is speculative in that we don’t really know for sure how the measles vaccine contributes to decreased non-measles-related mortality. We just know that, even after eliminating confounders, a beneficial effect remains. We also know that this these beneficial nonspecific effects (NSEs) might occur with other vaccines, as the authors of the current study note:
Previous studies have suggested that OPV might have beneficial NSEs (32, 35, 36). Findings from a randomized trial suggested that OPV might have beneficial non-specific effects that reduced all-cause mortality by 17% (30). Though the underlying biological mechanisms have not been fully studied, some studies suggest that OPV, just like BCG, is capable of inducing strong immune training (36). In this study, the NID campaigns with OPV or MV might have reduced the effect of being MV-after-DTP3 vaccinated vs MV-unvaccinated.
As has been shown for BCG, beneficial NSEs may be due to epigenetic changes reprogramming innate immunity. This may change once the child gets a new vaccination (19, 20). The specific immunological mechanisms behind the non-specific effects of vaccine are still being investigated, and it might be a mixture of heterologous immunity, trained innate immunity, and other types of changes in the immune system (16, 19).
The irony, of course, is that antivaxers frequently (and loudly) claim that vaccines harm the immune system when, if these hypotheses hold up, it would appear that exactly the opposite could well be the case. Vaccines actually do “stimulate the immune system” in beneficial ways, and those benefits could well go beyond just preventing the diseases intended to be prevented. They might even prevent type I diabetes, too.